Corrected Claims for Newly Eligible 65+ MMC Patients - $1.3M Issued in Cycle 2471
As of January 1, 2024, a new patient population aged 65 and older became eligible for Medicaid Managed Care. However, some health centers experienced issues receiving wrap and shortfall (CORC) payments for these patients.
CHCANYS has been actively working with DOH to address these concerns and help DOH identify the issue in eMedNY. As a result, they corrected over 10,000 claims, issuing payments totaling over $1.3 million, which are included in health centers’ Cycle 2471 Medicaid checks.
Since these claims were originally incorrectly denied, many health centers resubmitted them. As a result, you may notice a number of denied claims for duplicate billing in this remittance, along with the corrected payment for each date of service.
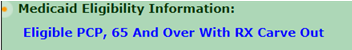
To determine if a patient is part of this new eligible population, ePACES will display "65 and over with RX carve-out." Health centers are entitled to receive their PPS rate for these patients, as well as wrap and shortfall (CORC) payments.
For more information on this new eligible population, refer to DOH's guidance.
